Tafida Raqeeb: Who decides the care of sick children?
The parents of five-year-old Tafida Raqeeb, who is on life support, have won permission to take her abroad for treatment.
So, why did the family have to go to court to decide what care she receives?
What's happened in Tafida's case?
Tafida Raqeeb suffered a traumatic brain injury in February as a result of a rare condition. She has arteriovenous malformation, where a tangle of blood vessels with abnormal connections between the arteries and veins risks causing a ruptured vessel.
Tafida's mother, Shelina Begum, and her father, Mohammed Raqeeb, wanted to seek treatment in Italy. But the Royal London Hospital, which is caring for their daughter, said releasing her was not in her best interests.
A spokesperson for Barts Health NHS Trust, which runs the hospital, said that its clinicians and independent medical experts had found "further medical treatment would not improve her condition".
It said it was in Tafida's best interests to withdraw treatment.
Can hospitals overrule parents?
In England and Wales the concept of parental responsibility is set out in law, in the Children Act 1989. This gives parents the responsibility broadly to decide what happens to their child, including the right to consent to medical treatment.
But this right is not absolute.
If a public body considers that a parent's choices are not in the best interests of their child, and an agreement cannot be reached, it can challenge these choices by going to court.
A judge makes the final decision, based on the evidence available.
The law does not consider either doctors or parents to be automatically right - instead, it says that the best interests of the child are the deciding factor.
A judge will have heard evidence about Tafida's clinical condition, the impact of moving her and the possibility of further treatment having any success, in order to decide the best course of action.
At the High Court, Mr Justice MacDonald said "life-sustaining treatment" for Tafida must continue. He dismissed Barts NHS Trust's application to withdraw life support.
Has this happened before?
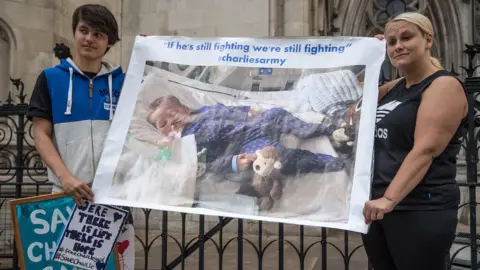 Getty Images
Getty ImagesTwo recent high-profile cases - of babies Charlie Gard and Alfie Evans - also tested the limits of parents' rights to decide what happens to their sick children.
Unlike the case of Tafida, both sets of parents lost their cases and were not able to move their children abroad for treatment.
Charlie was born on 4 August 2016 with an exceptionally rare genetic condition called encephalomyopathic mitochondrial DNA depletion syndrome (MDDS) which left him with severe brain damage, partial paralysis and unable to breathe unaided.
His parents wanted to take him to the US for experimental treatment, but the hospital treating him felt his life support should be switched off and he should be allowed to die with dignity.
Charlie's case eventually reached the highest UK court, the Supreme Court, which ruled that it was likely that Charlie would "suffer significant harm if his present suffering was prolonged without any realistic prospect of improvement".
His parents applied to appeal this decision in the European Court of Human Rights - which is not part of the EU. The European court said it would defer to the decision of the UK court, and ruled the appeal inadmissible.
Charlie died days later.
In the case of Alfie, there was no suggestion of new treatment - his parents wanted to transfer him to a hospital in Italy in order to prolong his life on ventilation.
He had a degenerative neurological condition and had been in a semi-vegetative state for most of his life.
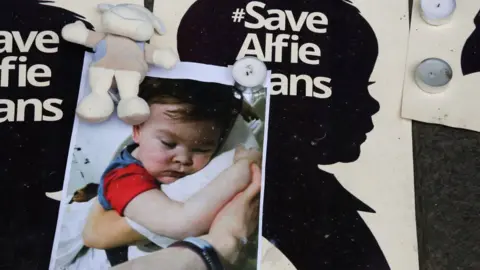 Getty Images
Getty ImagesAlfie died at the age of 23 months after a judge ruled that doctors could stop providing life support, against his parents' wishes,
In Tafida's case, the lawyer representing her family said there was "no evidence" she would suffer pain or harm from being moved.
But the NHS trust had said further treatment would be "invasive" and "futile".
Could things change?
At the moment, medical teams can lawfully refuse treatment if they can prove it is not in a child's best interests.
Charlie's parents are campaigning for a change in the law which they have dubbed Charlie's Law. They want doctors to have to prove a child would be at risk of "significant harm" as a result of the treatment.
This test is already used in other areas of child law, for example if a local authority applies to the courts to remove an at-risk child from its parents.
Charlie's mother, Connie Yates, says she also wants mediation to be provided to help doctors and parents come to a decision together without going to court.



