Covid: 'Israel may be reaching herd immunity'
 Getty Images
Getty ImagesA leading Israeli doctor believes the country may be close to reaching "herd immunity".
This happens when enough of a population has protection against an infection that it stops being able to spread - and even people who don't themselves have immunity are indirectly protected.
For Covid the estimated threshold for herd immunity is at least 65%-70%.
But scientists in the UK are more cautious.
Dr Sarah Pitt, a virologist at the University of Brighton, urged "extreme caution" in concluding that herd immunity had been reached - something she believes will be difficult even at high vaccination rates.
She said it was still too early to tell: "We need to see whether the cases in Israel continue to fall and stay at low levels."
Reaching this level of population immunity is important to protect people who can't be vaccinated or whose immune system is too weak to produce a good, protective response.
In Israel, more than half (5.3 million) its residents have been vaccinated and an additional 830,000 people have tested positive for the virus in the past, which should give them some natural immunity.
That works out as roughly 68% of the population who are likely to have antibodies in their blood which can fight off the virus.
Prof Eyal Leshem, a director at Israel's largest hospital, the Sheba Medical Center, said herd immunity was the "only explanation" for the fact that cases continued to fall even as more restrictions were lifted.
"There is a continuous decline despite returning to near normalcy," he said.
"This tells us that even if a person is infected, most people they meet walking around won't be infected by them."
And cases are falling in all age groups including children, even though under-16s are not generally being vaccinated.
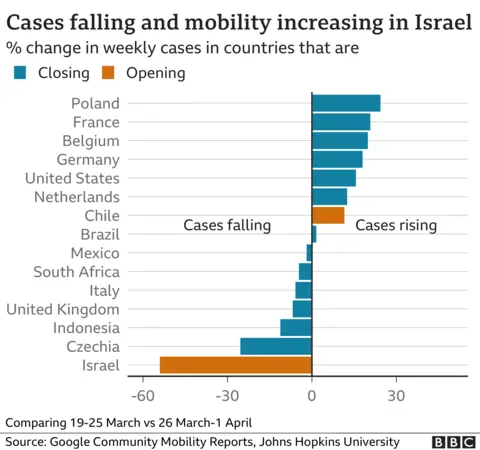
Google data reflect that many countries remained under lockdown as of the start of the month, with Israel and Chile two notable exceptions.
But unlike in Chile, as Israel opens up and people move around far more, cases have continued to decline.
How does herd immunity work?
Experts think that with no restrictions in place, someone infected with the original strain of the virus that causes Covid-19, will infect, on average three to four other people.
If it's three, then, in theory, once two-thirds of the population becomes immune to the virus, an infected person will, on average, only pass it to one other person. That's enough for the virus to spread, but not enough for it to grow.
You've eliminated two of those three people from the chain of transmission.
It sounds simple on paper. In reality, though, it's a little more complicated.
The vaccines are not 100% effective, and even when they stop people from getting sick they don't completely block infections in everyone.
That means some vaccinated people might still be able to pass on the virus.
Not everyone with a past Covid infection has strong or long-lasting natural immunity, and newer variants of the virus are more transmissible.
This means we may have to inoculate many more people before we reach that magic threshold.
But it's not all bad news. "I would say that we should not be looking for 'herd immunity' alone as a sign that we can lift all public health measures and get back to 'normal'," Dr Pitt explained.
"Rather we should be looking for consistently low levels of Covid-19 infection".
Is the UK close to herd immunity?
The UK is likely to be a way off this milestone - if it is ever reached.
Only about half the population had Covid antibodies, either from infection or vaccination, as of mid-March, according to the Office for National Statistics - though this will be higher now.
Remember it takes some time after being vaccinated for antibodies to build.
But the country is already starting to see the impact of vaccination on hospitalisations and deaths, with the biggest declines seen in the most vaccinated age groups.
There have been big falls in infection and illness among younger people too which might suggest the vaccine is blocking some transmission - although lockdown will have had a major effect too.
After herd immunity, what's next?
So far, new variants don't seem to be resistant to vaccines.
But a future variant which does show resistance to the vaccine, Prof Leshem explained, could mean people have less protection and the country could dip below the herd immunity threshold.
This isn't insurmountable - it could be tackled with tweaks to the vaccine, as already happens with the annual flu jab.
It serves as an important reminder, though - even if Israel has reached herd immunity, and if the UK follows, this is not necessarily a permanent state.
We can look at what's happened with measles in recent years.
The virus was considered to have been eliminated in the UK, but the World Health Organization revoked this status in 2019 after a "marked increase" in measles cases driven by a fall in the proportion of vaccinated people.
Measles is highly contagious - each infected person infects roughly 15 other people - so vaccination coverage needs to be over 90% to prevent outbreaks.
Follow Rachel on Twitter
